Almanac: Local hospital helps COVID patients navigate the ‘long haul’

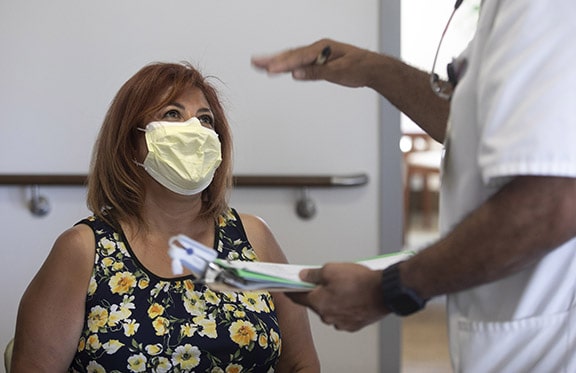
Pulmonary rehabilitation certified respiratory therapist Tammy Magill, checks a patient’s records recently at Pomona Valley Hospital Medical Center. Ms. Magill manages the Post COVID Recovery Program at the hospital which helps people who have COVID-19 symptoms months after initially recovering from the illness. COURIER photo/Steven Felschundneff
by Steven Felschundneff | steven@claremont-courier.com
Early in December 2020 Alta Loma resident Denalonor Bustamante had a sinus headache that would not go away. Although she telecommutes, she called in sick and was certain her symptoms would pass. The headache and sinus pressure became worse, until finally on December 9, her adult daughter became concerned and took her to Pomona Valley Hospital Medical Center’s emergency room. She was diagnosed with pneumonia and a sinus infection and was admitted. Ms. Bustamante spent the next 22 days in the hospital’s telemetry unit battling COVID-19.
“It was kind of strange,” Ms. Bustamante, 62, said. “I went in with a sinus headache and was diagnosed with pneumonia. The next day they said I tested positive for COVID.”
Ms. Bustamante has no idea how she contracted the coronavirus. Her family exercised extreme caution throughout the pandemic and she worked from home, rarely going out. Her husband Edward did most of the shopping so perhaps he contacted the virus at the grocery store. He, too, became sick but had a mild case.
Ms. Bustamante was hospitalized at the beginning of the winter COVID-19 surge, which complicated her treatment due to the many patients with the coronavirus. The doctors wanted to admit her to the intensive care unit but it was full. She was never intubated but was on high flow oxygen due to extreme shortness of breath.
To be discharged, Ms. Bustamante needed to reduce her dependence on the supplemental oxygen. “I worked really hard on my breathing so I would not be so reliant on the oxygen. By the grace of God I got [the oxygen] down,” she said.
But there was one last hurdle—she was going to need oxygen once she was home but it was in very short supply. She spent two very difficult days, technically well enough to go home but stuck in the hospital while the oxygen supply was located. Finally, through some advocacy of her own, Ms. Bustamante’s husband went to the medical supply center to retrieve the in-home oxygen unit and she was finally able to go home.
She was discharged on New Year’s Eve, which had been her goal all along because her daughter Amber was turning 21 that day and Ms. Bustamante wanted to be with her.
Once back at home she discovered new struggles. That first day she wanted more than anything to shower, but the bathrooms in her two-story home were upstairs. It took 45 minutes with a walker and the help of her family to get from the ground floor, up 13 steps and into the tub.
“The first couple of weeks at home, I was weak and slept all the time. My head and body ached—and I would cough nonstop for periods ranging from 45 minutes to two hours,” Ms. Bustamante said. “I had developed pulmonary thrombosis—my doctor described it as ‘taking shards of glass and spreading it on my lungs.’”
As time passed, Ms. Bustamante’s recovery stalled. In addition to the shortness of breath and fatigue, she experienced cognitive difficulty. A healthy and active woman before COVID, she now took 12 medications. Her doctors discovered she was diabetic.
Ms. Bustamante is one of a growing number of people struggling with a coronavirus complication known as long COVID or post-COVID syndrome, informally know as long haulers. Common symptoms include fatigue, difficulty thinking, loss of smell or taste, difficulty breathing, fast-beating or pounding heart, cough, joint or muscle pain, fever, depression and anxiety. According to a study published in the JAMA Journal, 10 percent of people who had only a mild case of COVID-19 experienced at least one moderate or severe symptom during the eight months following initial recovery. Pomona Valley’s website states 10 to 30 percent may have the syndrome.
Denalonor’s pulmonologist, Dr. Rakesh Sinha, soon referred her to Pomona Valley Hospital Medical Center’s Post-COVID Recovery Program managed by pulmonary rehabilitation certified respiratory therapist, Tammy Magill. Ms. Bustamante began twice-weekly sessions on February 18, which continue to this day.
Ms. Bustamante differs from most long COVID patients because she is middle aged and had a serious case of COVID-19. Most people who end up with protracted symptoms initially had mild cases and tend to be young and healthy. What is most troubling about post-COVID syndrome is no one knows whether, for some patients, it will be a chronic illness that will hamper their physical freedom for life.
“Interestingly, many of our Post-COVID Recovery Program patients were not necessarily the most ill, or those hospitalized the longest,” Ms. Magill said. “They managed their initial symptoms at home and, either never got over them completely, or got over them originally and symptoms returned months later.”
Ms. Magill leads a skilled multidisciplinary therapy team working to evaluate symptoms, test each patient’s underlying physiologic impairments, and individualize treatment plans. The goal is to help patients recover from the continuing effects of the disease through specialized therapies and progressive exercise programs designed to improve lingering symptoms and restore functional independence for each person as quickly and safely as possible, according to a news release from the hospital.
During a recent Wednesday afternoon Ms. Bustamante ambled into the rehabilitation room where she has her twice weekly sessions. She no longer needs supplemental oxygen during the day or a walker. She greeted Ms. Magill, and sat down to have her blood pressure taken by physical therapist Jerry Harris, who also provided a vital sign monitor for her finger.
Her session began with walking on a treadmill, followed by an arm strength machine that works like pedaling a bike with one’s hands, and finally, a stint on a recumbent bicycle machine.
“When I started here, I was on the treadmill and I barely made three minutes and I felt like I had run a marathon. I was gasping and could hardly breathe and that was with oxygen on,” Ms. Bustamante said. “Slowly we worked my oxygen level down and now I am at 20 minutes [on the treadmill] and my stamina has picked up.”
Ms. Magill and her team have helped over 150 patients since February, when the medical professionals were no longer needed for the surge in new COVID cases. They hit the ground running, seeing 10 new patients per week, 95 percent of whom have post COVID-19 syndrome.
In addition to the breathing issues, many people who enter the program have muscle atrophy from lying in bed for weeks. The physical therapy wakes those muscles up but can also result in cramping and a burning sensation. Loss of eyesight from macular degeneration and tightness in the chest are more common side effects of long COVID. Ms. Magill said anyone who experienced even a mild case of COVID-19 should see a cardiologist.
“Patients ask ‘how long will this last?’ but [she tells them] ‘I can’t give you a timeline because I don’t know,’” Ms. Magill said. “I am 32 years in respiratory therapy and have never seen anything like this. It is mind boggling.”
However, she has seen a tremendous positive change in many of the patients who are getting back to work, doing chores at home or driving again—basically moving on to their new normal.
“It’s been great,” Ms. Bustamante said. “When I started, Tammy was so very personable and attentive to me and made sure that I did not overdo it, because she saw that I would push myself.”
Ms. Bustamante continues to recuperate, but misses some of the hobbies she loved before her illness, like baking cakes. She most looks forward to riding bicycles with her husband Edward again.
“I almost feel normal again, it’s just difficult to breathe. I never thought I would have a hard time, we take it for granted how easy it is to breathe but I had to relearn how to breathe.”






0 Comments