COVID cases across LA County begin to stabilize
by Steven Felschundneff | steven@claremont-courier.com
Community spread of the coronavirus across all areas of the county has been in a sustained but slow decline over the past month, according to Barbara Ferrer, director of the Los Angeles County Department of Public Health.
Additionally, the county has satisfied five out of six state mandated COVID-19 benchmarks that must be met before schools and many businesses can reopen.
The county will not be removed from the state’s monitoring list until it can cut the two-week average of new cases from the current 295 infections per 100,000 residents to 100 cases or fewer.
As of Thursday, 38 of the 58 counties in the state were on the monitoring list, according to data provided by the California Department of Public Health.
In Claremont there has been a sharp increase in the number of reported cases in the city’s unincorporated areas, from four to 17 in a matter of days. Unincorporated Padua Hills is reporting three people with COVID-19, bringing Claremont’s cumulative cases to 339, with eight deaths.
There was no further information about the sudden change in unincorporated Claremont and, unfortunately, the county only provides details on outbreaks when they happen in an institutional setting.
Claremont Manor and its care center have combined cases of 12 staff, four residents and one death as of Thursday morning. Claremont Place remains at two staff and one resident. Mt. San Antonio Gardens reports eight staff members and 10 residents are postive, with one death.
Mountain View Center in Claremont now has five residents testing positive. Western Assemblies Home still reports 13 staff, six residents and one death.
Pilgrim Place is still reporting no cases of COVID-19 among residents or staff members.
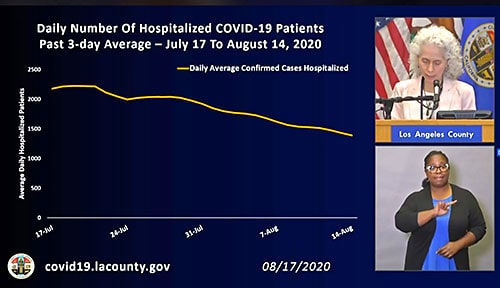
Ms. Ferrer identified daily hospitalizations, case rate and positivity rate as the three key indicators that the virus spread is slowing.
Over the past month the three-day average of hospitalizations has decreased steadily from 2,219 people hospitalized on July 17 to 1,378 on August 19, a 37 percent change. She said the declining hospitalization rate is a particularly good sign because that data reflects how many people are currently seriously ill.
Although cases are down, the data is not complete due to the backlog created several weeks ago by the state of California’s electronic laboratory reporting system. However, the trajectory is still moving lower—in mid July average daily new cases were around 3,200 but by mid August that had fallen to about 2,000. Over that same period of time the positivity rate has fallen from over 10 percent to just above six percent.
In spite of the uncertainty created by the state’s ELR glitch the data is spread over many days, even weeks, so public health officials anticipate that this decrease will hold.
“I hope this data reminds all of us of the power our actions have in preventing serious illness and saving lives, and again I want to just say how grateful I am for everyone who’s doing their part to make sure we slow the spread of COVID-19,” Ms. Ferrer said. “We do still have a way to go to reduce community transmission enough to be able to have confidence that the timing would be right to reopen our schools and get more people back to work.”
During a news conference Monday Ms. Ferrer reiterated how dangerous it is for people to gather socially with others who are not part of the immediate family one lives with. She cited reports of gatherings for parties, weddings and other celebrations that have resulted in participants unknowingly infecting other attendees.
“We have many examples here in our county and across the country of gatherings, parties and services that did result in outbreaks of COVID-19,” Ms. Ferrer said. “We’ve seen outbreaks from gatherings on college campuses, fraternity and sorority houses, restaurants, from our protests, churches and at people’s homes all across the country, and some of these gatherings have resulted in tragic loss of life and serious illness.”
Ms. Ferrer closed on a positive note, thanking all of the people across the county who have stayed home, worn a face covering and practiced social distancing.
“We know from the past that when we work together we slow the spread and it seems we have done just that again,” she said.
Since its first report in early March, public health has identified 225,827 cumulative cases of COVID-19 across all areas of LA County, and 5,392 deaths. In a news release Wednesday the county reported 1,956 new cases and 61 deaths.
Data continue to show that Latino and Black residents are dying at rates far higher than those for white residents—however, signs of progress toward closing the gaps are emerging.
At the peak of community transmission in mid July, Latinos were six times more likely to die from COVID-19 than whites. Today that has been reduced significantly, though Latinos are still 2.5 times more likely to die as a result of the virus.
In July, Black residents had a death rate three times higher than whites, but by mid August the rate had improved to the point where it is only slightly higher for Blacks.
Income disparity is an even bigger indicator of death risk, particularly among people living in low income neighborhoods. During the peak, low income residents were seven times more likely to die as a result of COVID-19. There has been improvement in this demographic as well, however, low income people are still 4.6 times more likely to die from the virus.









0 Comments